By Tara Dillion, CNP
Central Ohio Geriatrics
What Is Vitamin D?
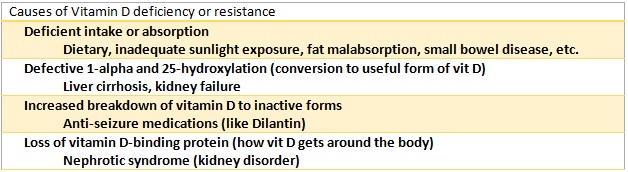
Vitamin D, also known as calciferol, is actually a generic term for a group of fat-soluble compounds. It’s the vitamin we tend to associate with bone health, and indeed, bone metabolism is one of its primary clinical roles. Vitamin D is biologically inactive until converted in the liver and kidneys to an active metabolite the body can use. Thus, there are several ways someone can develop vitamin D deficiency, either because they don’t get enough, can’t use it, and/or can’t store it.
Why is vitamin D important?
Vitamin D levels have a direct effect on other hormone levels, particularly parathyroid hormone (PTH). Patients who have low vitamin D levels can have high PTH levels, leading to accelerated bone loss which can cause bone fractures. Muscle strength and balance are also affected, making pain, weakness and falls more likely. Research continues on more potential benefits of adequate vitamin D levels, including improvements in cardiovascular and immune systems.
So where do I get vitamin D?
We can get vitamin D from dietary intake or production in our skin when exposed to sunlight. Some foods (like cereals, bread, and milk) are fortified with vitamin D, but why? There are very few foods that naturally contain vitamin D, so unless you regularly dined on fatty fish livers, sunlight would be your major source of vitamin D. Unfortunately, several factors keep our skin from producing enough vitamin D. Infants, disabled persons, and the institutionalized may not spend enough time outdoors to get sun exposure. In central Ohio, particularly during the winter, there is simply not enough radiation from the sun to convert vitamin D in our skin, regardless of the amount of time spent outside. Since we can’t rely on regular sun-derived vitamin D production, dietary fortification helps meet our daily requirements.
How do I know if I need more vitamin D?
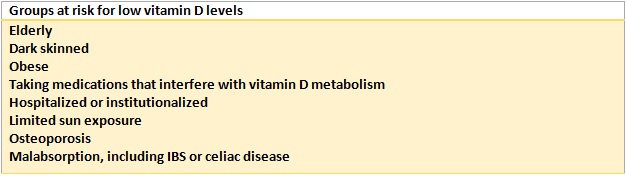
Vitamin D levels are most often checked with a blood test called serum 25(OH)D. Testing everyone for low vitamin D levels would be expensive and unnecessary. Instead, testing is done based on risk factors that make a patient more likely to have low vitamin D.
Experts disagree on what level of vitamin D is ideal, some say 20-40 ng/mL, others say 30-50 ng/mL. The American Geriatric Society recommends older adults have levels at least 30 ng/mL to minimize risk of fall and fracture. The prevalence of vitamin D deficiency is difficult to measure, but it seems to be a common problem. One national survey reported over 41% of adults with 25(OH)D levels below 20 ng/mL.
Can I have too much vitamin D?
There’s also some disagreement (and frankly, a lack of data) regarding the safe upper limit of vitamin D levels. While there is plenty of evidence regarding the potential danger of low vitamin D levels, this isn’t a case of “more is better”! Past studies and guidelines have raised flags with levels above 50 ng/mL, though it’s unclear if the observed increase in mortality was due to the original vitamin D deficiency or the replacement afterwards. The first measurable toxicity concerns (high calcium levels) start when levels are over 88 ng/mL, which usually applies only to those taking “megadose” supplements on a fad diet or because of malabsorption issues. Symptoms of toxicity include confusion, loss of appetite, vomiting, muscle weakness, extreme thirst, and excessive urination. By the way, you can’t get toxic vitamin D levels by “overdosing” on sunlight. The melanin your skin produces in response to sun exposure reduces production of vitamin D, and your skin converts the extra vitamin D to inactive forms. You can get a bad sunburn, though, so this isn’t an excuse to forget your sunscreen!
So how much vitamin D is just right?
We won’t get into recommendations for infants, children, and pregnant women, but most adults who don’t have regular, year-round sun exposure should take 600-800 international units (IUs) of vitamin D daily. The American Geriatric Society and National Osteoporosis Foundation recommend up to 1000 IUs for older adults to reduce risk of falls and fractures. If your primary care provider tests your blood and finds you have low vitamin D levels, they may prescribe a higher dose for you. Vitamin D supplements are generally in one of two forms, vitamin D3 (cholecalciferol) or vitamin D2 (ergocalciferol). Vitamin D3 has a higher affinity for the vitamin D-binding protein, meaning it raises blood levels more efficiently than D2. You may be prescribed doses to be taken daily, weekly, or monthly. For those with levels <20 ng/mL, a commonly used regimen is 50,000 IUs of vitamin D3 weekly for 8 weeks, then a maintenance dose of 1000-2000 IUs daily. Higher or lower doses may be required depending on your body’s ability to absorb and store the vitamin D. Some providers recheck 25(OH)D levels 3-4 months after starting supplementation and adjust the dose accordingly.
Questions?
Talk to your primary care provider or geriatrician for more information about your personal health needs.
References:
Dawson-Hughes, B. (2015). Vitamin D deficiency in adults: Definition, clinical manifestations, and treatment. In J.E. Mulder (Ed.), UpToDate.
Holick, M.F. (May 2015). Vitamin D is not as toxic as was once thought: a historical and an up-to-date perspective. Mayo Clinic Proceedings, 90(5), 561-4.
Pazirandeh, S. & Burns, D.L. (2015). Overview of vitamin D. In J.E. Mulder (Ed.), UpToDate.